Mental health has, in recent years, become increasingly recognized in many communities. More than 21% of adults across the United States received mental health care in 2021, according to a report released by the CDC. Furthermore, the younger generation is gradually becoming more comfortable discussing mental health.
Now, people are more likely to pursue treatment for mental health disorders. They may openly discuss mental health conditions and challenges, both among friends and family members and the workplace. As the stigma gradually continues to lift, many people can better receive diagnosis and treatment for serious mental health conditions.
Unfortunately, some communities remain underrepresented when seeking the mental health care they need, often because of a built-in stigma against mental health care and everything it represents.
People are more likely to receive the mental health care they need when it is accepted in their communities. When others around them embrace mental health support, resources are readily available, and people are willing to break the silence and talk about mental health. In South Asian communities, there is a strong taboo against speaking about mental health. As a result of the mental health stigma, many people go untreated.
With just over 400 trained psychiatrists for a population exceeding 220 million, Pakistan faces a significant gap in mental health care. Non-profit organizations like Taskeen are working to fill this gap by offering mental health education and resources, aimed at reducing the stigma and facilitating access to professional help.
Bangladesh, a densely populated country, has a relatively higher prevalence of mental health disorders. The government, recognizing the necessity of mental health, has incorporated it into their health care policies, with the National Mental Health Act (2018) being a landmark step towards ensuring mental health services.
Sri Lanka’s mental health landscape is marked by the impact of its civil war. The government and NGOs are working together to provide psycho-social support to affected communities, highlighting the need for trauma-informed mental health care.
Natural disasters like the devastating 2015 earthquake have had a significant impact on Nepal’s mental health situation. Organizations like TPO Nepal are focusing on providing mental health and psychosocial support in post-disaster situations.
Dealing with intrinsic reluctance to seek care for mental health concerns can make it very difficult for people suffering from depression or anxiety to seek treatment for those mental health conditions.
Often, patients worry about the stigma associated with seeking care. Their parents and other members of older generations might insist that they should not have those challenges. People who are struggling may be encouraged to push past their mental health challenges.
As a result, even younger people who may have started to shift away from the intrinsic bias against mental health care may be reluctant to seek treatment or stick to a treatment protocol they might have to share with others.
Children may also be reluctant to share mental health symptoms with parents and other family members. Despite the need for care to help overcome those symptoms, children may choose instead to keep them to themselves out of fear of the stigma attached to them. Even when they report symptoms to their parents, children may not be given treatment options or support and may instead have their concerns brushed aside.
Among older members of South Asian communities, there is often a general lack of awareness regarding mental health symptoms. In many cases, members of those communities may fail to recognize the presence of even severe mental health symptoms and warning signs due to a lack of overall awareness of those symptoms. While younger people in South Asian communities are now more likely, in general, to discuss mental health, their parents and other adult members of the family may not fully recognize the symptoms in front of them.
South Asian parents may also prove less likely to recognize warning signs of serious mental health conditions in their children. That may mean that they miss signs of things like:
Sometimes, even with a mental health condition identified, members of South Asian communities may show a generalized resistance to treatment. South Asian parents, for example, may show reluctance to treat their children “because of what others might think,” especially if they worry about identifying that treatment to other community members.
There may also be a general fear that the family will end up bearing the weight of the diagnosis: that others will notice that the family cannot make one member happy, increasing overall depression, for example. Even when families bring their children in for counseling, they may not be willing to seek appropriate treatment for any diagnosis they might receive.
Mental illness is often hereditary. While the fact that a family member has a mental health condition does not necessarily mean that others will develop it, it can increase the likelihood. Children with parents with specific mental health conditions may be more likely to develop those symptoms themselves.
In South Asian families, however, many family members will not address those conditions. Parents with ADD or ADHD may not identify their symptoms and may continue to struggle with them all their lives. Unfortunately, this may also mean that when children start showing signs of ADD or ADHD, parents simply expect them to manage those symptoms independently. Rather than providing children with the support they may need to overcome those diagnoses.
Parents may also think those mental health symptoms are “normal” or “something everyone goes through.” This may be particularly true in cases of hereditary mental illnesses, where many family members may show the same general symptoms.

Across the course of their lifetimes, at least 1 in 5 South Asians report a mood or anxiety disorder. The actual rate of those disorders may be higher thanks to self-reporting and a lack of identification of key symptoms of those mental health conditions.
Around 19% of adults across the United States seek treatment for anxiety-related conditions each year. Assuming the same rate of occurrence within the South Asian community, that may mean that a high percentage of South Asians suffering from mental health conditions, including anxiety, go without treatment each year.

While South Asian men may generally shower fewer drinking behaviors when they do drink, they often have a greater likelihood of struggling with heavy drinking. In one study, 24% of South Asian men surveyed reported an episode of heavy drinking within 30 days of the survey. 64% of those surveyed reported drinking within the same period.
Many people use alcohol to help self-medicate for various mental health conditions. Drinking can, temporarily, seem to alleviate symptoms of anxiety or make them easier to handle. Unfortunately, drinking can also increase the risk of depression and exacerbate the presentation of many mental health conditions.
Furthermore, heavy drinking may interfere with processing several types of medications used to treat common mental health conditions. Sometimes, drinking may make those drugs more effective, which means that they can increase the symptoms of intoxication or that drinking may cause those drugs to process through the system faster, leaving overall gaps in treatment periods. In other cases, heavy drinking may prevent the medications from working or absorbing, leaving the patient feeling as though they have received no treatment for those conditions.
In many cases, members of the South Asian community will be less likely to seek treatment for mental health conditions, even after diagnosis. Among Asian Americans with a diagnosed psychiatric disorder, only around 40% of American-born individuals reported using mental health services. Only 23% of those born outside the United States took advantage of those services.
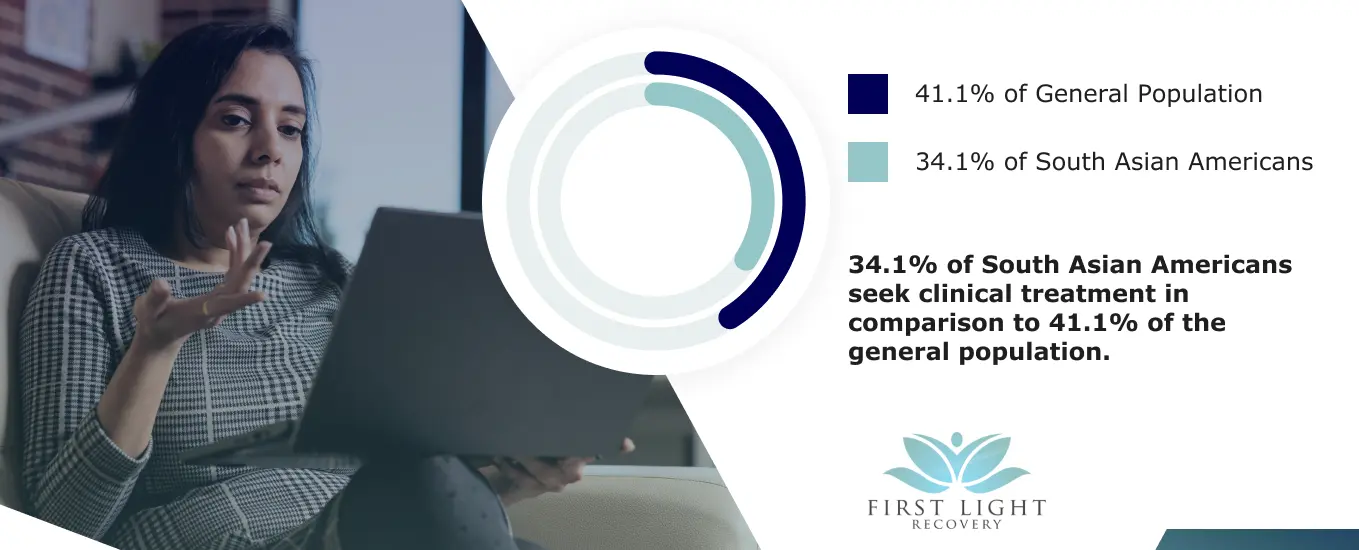
Asian Americans may also be less likely to seek mental health care within 12 months, even when presenting with serious symptoms of a possible mental health condition. Across the United States, around 41.1% of the general population reports pursuing care within a year of establishing the presence of symptoms. Only 34.1% of South Asian Americans sought treatment.
In the United States, suicide is the twelfth leading cause of death. However, suicide rates are significantly higher than the average in the Asian American community. Unfortunately, people under severe mental health pressure may prove more likely to commit suicide when they cannot pursue treatment or do not have a reasonable treatment option.
A persistent lack of acceptance from family members, including the “all in your head” mentality or “get over it,” can continue eroding mental health. In some cases, mental health can be strained to the point that suicide becomes more likely. Instituting proper mental health support within the South Asian community in the United States can help decrease suicide rates and improve overall mental health.
Having the proper support to overcome mental health conditions is critical, whether you need to pursue counseling, medication, or a combination of treatment methods. At First Light Recovery, we offer mental health resources and support for ADHD, anxiety, bipolar disorder, BPD, depression, impulse control disorder, obsessive-compulsive disorder, PTSD, schizoaffective disorder, schizophrenia, social anxiety, and suicidal ideation.
Contact us today to learn more about how we can support members of the South Asian community and others on their mental health journey.
If you’re struggling with your mental health, you don’t have to face it alone. First Light Recovery offers compassionate care, expert treatment, and a real-world approach to empower you.
© 2025 First Light Recovery. All rights reserved.
First Light Recovery
We firmly believe that the internet should be available and accessible to anyone, and are committed to providing a website that is accessible to the widest possible audience, regardless of circumstance and ability.
To fulfill this, we aim to adhere as strictly as possible to the World Wide Web Consortium’s (W3C) Web Content Accessibility Guidelines 2.1 (WCAG 2.1) at the AA level. These guidelines explain how to make web content accessible to people with a wide array of disabilities. Complying with those guidelines helps us ensure that the website is accessible to all people: blind people, people with motor impairments, visual impairment, cognitive disabilities, and more.
This website utilizes various technologies that are meant to make it as accessible as possible at all times. We utilize an accessibility interface that allows persons with specific disabilities to adjust the website’s UI (user interface) and design it to their personal needs.
Additionally, the website utilizes an AI-based application that runs in the background and optimizes its accessibility level constantly. This application remediates the website’s HTML, adapts Its functionality and behavior for screen-readers used by the blind users, and for keyboard functions used by individuals with motor impairments.
If you’ve found a malfunction or have ideas for improvement, we’ll be happy to hear from you. You can reach out to the website’s operators by using the following email
Our website implements the ARIA attributes (Accessible Rich Internet Applications) technique, alongside various different behavioral changes, to ensure blind users visiting with screen-readers are able to read, comprehend, and enjoy the website’s functions. As soon as a user with a screen-reader enters your site, they immediately receive a prompt to enter the Screen-Reader Profile so they can browse and operate your site effectively. Here’s how our website covers some of the most important screen-reader requirements, alongside console screenshots of code examples:
Screen-reader optimization: we run a background process that learns the website’s components from top to bottom, to ensure ongoing compliance even when updating the website. In this process, we provide screen-readers with meaningful data using the ARIA set of attributes. For example, we provide accurate form labels; descriptions for actionable icons (social media icons, search icons, cart icons, etc.); validation guidance for form inputs; element roles such as buttons, menus, modal dialogues (popups), and others. Additionally, the background process scans all the website’s images and provides an accurate and meaningful image-object-recognition-based description as an ALT (alternate text) tag for images that are not described. It will also extract texts that are embedded within the image, using an OCR (optical character recognition) technology. To turn on screen-reader adjustments at any time, users need only to press the Alt+1 keyboard combination. Screen-reader users also get automatic announcements to turn the Screen-reader mode on as soon as they enter the website.
These adjustments are compatible with all popular screen readers, including JAWS and NVDA.
Keyboard navigation optimization: The background process also adjusts the website’s HTML, and adds various behaviors using JavaScript code to make the website operable by the keyboard. This includes the ability to navigate the website using the Tab and Shift+Tab keys, operate dropdowns with the arrow keys, close them with Esc, trigger buttons and links using the Enter key, navigate between radio and checkbox elements using the arrow keys, and fill them in with the Spacebar or Enter key.Additionally, keyboard users will find quick-navigation and content-skip menus, available at any time by clicking Alt+1, or as the first elements of the site while navigating with the keyboard. The background process also handles triggered popups by moving the keyboard focus towards them as soon as they appear, and not allow the focus drift outside it.
Users can also use shortcuts such as “M” (menus), “H” (headings), “F” (forms), “B” (buttons), and “G” (graphics) to jump to specific elements.
We aim to support the widest array of browsers and assistive technologies as possible, so our users can choose the best fitting tools for them, with as few limitations as possible. Therefore, we have worked very hard to be able to support all major systems that comprise over 95% of the user market share including Google Chrome, Mozilla Firefox, Apple Safari, Opera and Microsoft Edge, JAWS and NVDA (screen readers).
Despite our very best efforts to allow anybody to adjust the website to their needs. There may still be pages or sections that are not fully accessible, are in the process of becoming accessible, or are lacking an adequate technological solution to make them accessible. Still, we are continually improving our accessibility, adding, updating and improving its options and features, and developing and adopting new technologies. All this is meant to reach the optimal level of accessibility, following technological advancements. For any assistance, please reach out to